Introduction
Welcome to the Baxter Healthcare Scheme guide.
Baxter have appointed us, Healix Health Services Ltd, to manage this scheme. Our role is to assess and manage medical needs that you might have as well as the care and treatment you receive.
The Baxter Healthcare Scheme is designed to cover you for the diagnosis and/or treatment of a short term medical condition, if the treatment is medically necessary.
The scheme is not intended to cover all medical conditions. There are some medical conditions and treatments that are excluded from cover (please see exclusions and limitations for further details on this).
All treatment (including consultations and diagnostic tests) should be authorised in advance. Therefore it is essential that you call us before you receive treatment, to ensure that your proposed treatment is eligible for cover under the scheme.
If you wish to include your partner or dependants under the scheme, regardless of their gender, please reach out to your HR department for guidance on eligibility.
Table of benefits
Your scheme benefits are set out in the table below.
All claims are subject to your excess, which will be applied to the first eligible treatment within each scheme year.
Benefit limits apply to each individual member in any one year of cover, unless otherwise specified.
Once any of your benefit limits are reached, there will be no further cover for this benefit until the scheme's annual renewal date unless otherwise specified.
The scheme will commence on the 1st January 2025 to 31st December 2025.
| Outpatient Investigations and Treatment | Level of cover | Benefit note |
Outpatient diagnostic tests, investigations and consultations with a specialist or practitioner following GP or specialist referral (self-referral available for specified cancer symptoms) |
Full cover | 1a |
Orthotics |
Up to £500 per scheme lifetime | 1b |
Outpatient treatment and surgical procedures |
Full cover | 1c |
Outpatient MRI, CT and PET scans following specialist referral |
Full cover | 1d |
Monitoring of a chronic condition |
Up to £1,000 per scheme year | 1f |
| Inpatient and Daycase Treatment | ||
Specialist fees and hospital charges for inpatient and daycase treatment |
Full cover | 2a |
Parent accommodation |
Full cover | 2b |
| Therapies | ||
In-network physiotherapy (including self-referral) |
Full cover | 3a |
Outpatient therapies following GP referral |
Up to 10 sessions per scheme year | 3b |
Outpatient therapies following specialist referral |
Full cover | 3c |
| Cancer Treatment | ||
Cancer treatment |
Full cover | 4a |
Cancer outpatient therapies Cancer alternative therapies (£250 limit within the £1,000 limit per scheme year) |
Combined limit of up to £1,000 per scheme year | 4b |
Cancer outpatient mental health treatment |
Up to £1,000 per scheme year | 4c |
Cancer additional services |
Full cover | 4d |
| Cash Benefits | ||
NHS cash benefit |
£300 per day or night | 5a |
NHS cash alternative |
Up to 25% of the costs to receive the procedure privately – please contact us to check if your procedure will be eligible | 5b |
NHS cancer cash benefit |
£300 per day or night | 5c |
NHS cancer cash benefit for oral chemotherapy and targeted therapies |
£600 per month | 5d |
| Additional Benefits | ||
Women's and Men's Health Benefit Remote advice service with our in-network experts (up to 4 consultations per scheme year) Diagnostic tests and investigations following referral from our in-network experts (up to £500 per scheme year) |
Limited cover | 6a |
Private ambulance charges |
Full cover | 6b |
Home healthcare |
Full cover | 6c |
Overseas emergency treatment |
Limited cover | 6d |
Note: The above benefits only apply when the covered person has treatment in the UK unless otherwise specified.
Outpatient investigations and treatment
We will pay in full for:
- outpatient consultations with a specialist following GP referral
- outpatient consultations with a dietician, nurse, orthoptist, podiatrist or speech therapist following GP or specialist referral. The practitioner must be registered with the correct governing body for their field, and meet our definition for a practitioner
- outpatient diagnostics and investigations following GP or specialist referral
Cover is subject to our reasonable and customary fees.
Outpatient consultations with a specialist on self-referral for specified cancer symptoms
We will pay in full for self-referred consultations and investigations for specified cancer symptoms.
Please refer to the self-referred cancer benefits page for further information on the symptoms that are eligible and how to access this benefit.
If a diagnosis of cancer is made, cover for eligible treatment will be subject to any limits as detailed in your cancer treatment benefit.
Back to topWe will pay up to £500 per scheme lifetime towards medically necessary orthotics, when these are recommended by a GP, practitioner, physiotherapist or specialist.
Back to topWe will pay in full for hospital charges and specialist fees for outpatient treatment, surgical procedures, and drugs and dressings used during an outpatient appointment.
Cover is subject to our reasonable and customary fees.
Back to topWe will pay in full for MRI, CT and PET scans following specialist referral.
Back to topWe will pay up to £1,000 per scheme year for the following when required to monitor a chronic condition:
- outpatient consultations with a specialist following GP referral
- outpatient diagnostic tests and investigations following GP or specialist referral
Once this benefit limit has been reached the chronic condition rule applies as detailed in your exclusions and limitations.
Back to topWe will pay for specialist fees for inpatient and daycase treatment. Cover is subject to our reasonable and customary fees.
We will pay hospital charges in full for the following:
- accommodation and nursing care for inpatient or daycase treatment
- operating theatre and recovery room
- prescribed medicines and dressings, for use whilst an inpatient or for daycase treatment
- eligible surgical appliances - for example, a knee brace following ligament surgery
- prosthesis or device which is inserted during eligible surgery
- pathology, radiology, diagnostic tests, MRI, CT and PET scans
- physiotherapy received during inpatient or daycase treatment
- intensive care
- short-term dialysis when needed temporarily for sudden kidney failure resulting from an eligible condition or treatment
- skin and corneal grafts
We will pay reasonable hospital costs for one parent or legal guardian to stay with a child who is under 16 years old, if a child is admitted to hospital as an inpatient. Cover for this benefit will stop on the child’s 16th birthday. If your child is an inpatient on their 16th birthday, then cover will extend until they are discharged on that occasion. We will only pay the cost if:
- it is the parent or legal guardian who stays with the child
- the treatment the child receives is covered by the scheme
We will pay in full for outpatient physiotherapy following GP, specialist or self-referral when treatment is provided by our physiotherapy network provider.
Please refer to the musculoskeletal pathway for further information.
Back to topWe will pay up to a combined limit of 10 sessions per scheme year for out of network physiotherapy, osteopathy, acupuncture and chiropractic treatment following GP referral. Treatment must be taken with a physiotherapist or complementary practitioner that we recognise for benefit purposes.
Back to topWe will pay in full for outpatient out of network physiotherapy, osteopathy, acupuncture, and chiropractic treatment following specialist referral. Treatment must be taken with a physiotherapist or complementary practitioner that we recognise for benefit purposes.
Back to topWe will pay for cancer treatment as detailed in the cancer cover explained table.
Please refer to cancer support explained for information on the additional supportive services available.
Back to topWe will pay up to a total limit of £1,000 per scheme year for the following therapies, when required as a direct result of eligible cancer treatment.
Cancer outpatient therapies on GP, specialist or self-referral
We will pay up to the benefit limit for physiotherapy, osteopathy, chiropractic treatment, manual lymphatic drainage and dietician services.
Treatment must be taken with a physiotherapist, practitioner or complementary practitioner that we recognise for benefit purposes.
Cancer alternative therapies on GP, specialist or self-referral
We will reimburse up to £250 on a pay and claim basis within the above combined limit of £1,000 per scheme year for acupuncture, reflexology and aromatherapy.
We will pay up to £1,000 per scheme year on GP, specialist or self-referral for outpatient mental health treatment required as a direct result of eligible cancer treatment.
Mental health treatment is only covered if it is provided by a psychological therapist or psychiatrist.
Back to topWe will pay in full for the cost of external prosthesis, wigs, scalp cooling treatment and medical tattooing for reconstructive purposes only when recommended by your specialist and required as a direct result of eligible cancer treatment.
For wigs and medical tattooing, this benefit is available on a pay and claim basis only.
Back to topIn the event that you are admitted to an NHS hospital, or you elect to receive free treatment through the NHS we will pay an NHS cash benefit of £300 per night or day, for inpatient or daycase treatment. This benefit will only apply to claims for daycase or inpatient treatment that would otherwise have been eligible for benefit under your scheme.
Back to topIn the event that you require an eligible elective surgical procedure, and you choose to receive this treatment free of charge on the NHS, we may pay you a cash lump sum. Please contact the claims helpline to check if your procedure will qualify for this benefit.
Back to topIn the event that you elect to receive free cancer treatment through the NHS, we will pay an NHS cancer cash benefit of £300 per night or day following eligible inpatient or daycase treatment, or outpatient radiotherapy treatment.
This benefit will only apply to claims for daycase or inpatient treatment that would otherwise have been eligible for benefit under your scheme.
Back to topIn the event that you elect to receive oral chemotherapy or targeted therapies via the NHS as an outpatient, we will pay an NHS cancer cash benefit of £600 per month whilst you receive such treatment.
Back to topRemote advice service with our in-network experts
We will pay for up to 4 remote advice appointments per scheme year with our in-network experts on self-referral. This service can be used to discuss any health concern including conditions that are normally excluded for cover such as the menopause, andropause, sexual health concerns, fertility or contraception advice.
Diagnostic tests and investigations following referral from our in-network experts
We will pay up to £500 per scheme year for diagnostic tests or investigations that are recommended following a remote advice appointment with our in-network experts.
Remote consultations and diagnostic tests and investigations will be covered up to the limits described above only. Once the benefit limits have been reached the scheme rules will apply as detailed in your exclusions and limitations.
Please note: additional cover may be available outside of the above limits for eligible claims, please contact the claims helpline for further information.
Please refer to the women's or men's health services page for further information on how to access these benefits.
Back to topWe will pay in full for transport by a private ambulance to and/or from a hospital when ordered for medical reasons.
Back to topWe will pay in full for home nursing charges for registered nurses when recommended by a specialist and where treatment is:
-
medically necessary and without it you would have to receive treatment as an inpatient or daycase admission
-
needed for medical reasons (i.e. not social or domestic reasons)
-
under the direct supervision of a specialist
Mental health treatment delivered at home or in the community is not covered by the scheme.
Back to topThe scheme is designed to cover treatment in the UK, and therefore provides limited cover for treatment you may require whilst abroad. We strongly recommend that you ensure you have adequate travel insurance and/or a European Health Insurance Card / Global Health Insurance Card in place before you travel abroad on holiday.
If you wish to claim for emergency treatment received abroad, you must send us proof of how long you were abroad for (this period should not exceed 28 consecutive days). You should also send us all medical bills and receipts associated with your treatment. Failure to submit receipts within six months of the date of treatment may result in the claim being denied.
We will reimburse reasonable and customary costs for overseas emergency treatment as detailed below:
| Treatment | Reimbursement level |
| Specialist fees | Within our reasonable and customary fees |
| MRI, CT and PET scans |
Up to £100 per trip |
| Outpatient surgical procedures | Up to £100 per trip |
| Other emergency outpatient treatment (excluding MRI, CT and PET scans, and outpatient surgical procedures) | Up to annual outpatient benefit limits, as detailed in the table of benefits |
| Inpatient or daycase surgical procedures | Up to £200 per trip |
We will only pay up to the above limits if the following apply:
-
the treatment is eligible for benefit
-
the treatment is carried out by a specialist who is:
-
fully trained and legally qualified and permitted to practice by the relevant authorities in the country in which your treatment takes place, and
-
is recognised by the relevant authorities in that country as having specialised knowledge of, or expertise in, treatment of the disease, illness or injury being treated; and
-
the treatment facility is specifically recognised or registered under the laws of the territory in which it stands for providing the treatment delivered
We will not pay for overseas emergency treatment in any country if:
-
the Foreign and Commonwealth Office has advised against travel to that country or area. If you are already in the country or area when the Foreign and Commonwealth Office advises against travel, and you require treatment, this should be claimed for under your travel insurance policy
-
you are already in that particular country or area and have been advised to leave unless prior written authority has been received from us. If you are unable to leave a particular country or area after being advised to do so, and you require treatment, this should be claimed for under your travel insurance policy
-
you travelled abroad despite being given medical advice not to travel abroad
-
you travelled abroad to receive treatment, or
-
the treatment you require is related to a pre-existing condition
The scheme will not pay for:
-
GP services or fees
-
outpatient prescriptions
-
take home drugs and dressings
-
any costs associated with an evacuation or repatriation
-
any treatment that should be free or provided at a reduced cost under a reciprocal agreement or EHIC/GHIC
Costs of private treatment in facilities in the European Union, Iceland, Liechtenstein, Norway or Switzerland or costs in state facilities in these countries which should have been free or reduced if you had had a European Health Insurance Card / Global Health Insurance Card are not covered under the scheme.
If you are a UK resident, you are entitled to medical treatment that becomes necessary, at reduced cost or sometimes free, when temporarily visiting a European Union (EU) country, Iceland, Liechtenstein, Norway or Switzerland. Only treatment provided under the state scheme (the country’s equivalent to the NHS) is covered. However, to obtain treatment you will need to take a European Health Insurance Card (EHIC) or Global Health Insurance Card (GHIC) with you.
EHIC are still valid if in date, but they have now been replaced by the GHIC. You can apply for a GHIC by clicking here.
Your scheme will not cover you for the costs of an evacuation or repatriation should you require this. Therefore we strongly recommend that you take out appropriate travel insurance if you are going abroad to ensure that you have adequate cover for any healthcare needs you have along with cover for loss of luggage etc.
Back to topCancer cover explained
We know that a cancer diagnosis is a life changing event and therefore understand that this is an important part of your medical scheme. To help you understand the level of cover available to you, this section gives more information about your cover for cancer.
The Baxter Healthcare Scheme provides benefit for active inpatient, daycase or outpatient treatment for a diagnosed malignancy. This includes surgery, radiotherapy or chemotherapy, alone or in combination. The scheme does not pay benefit where the treatment is preventative, for maintenance purposes, or where it continues indefinitely.
To ensure that you receive the highest quality of care at all times we identify centres of excellence for the treatment of cancer. If you are diagnosed with cancer we may require you to transfer to one of these centres. These centres may be either in the private or NHS sector.
Should you choose to receive eligible inpatient, daycase or outpatient treatment at an NHS centre you will be eligible for the NHS cancer cash benefit as shown on your table of benefits.
One of our nurse case managers will be able to provide information on the treatment options available to you and support you through your treatment.
| Summary of cancer benefits | What’s covered | What’s not covered |
| Where will I be covered to have treatment? |
You will be covered in full for eligible treatment:
|
You will not be covered for any treatment received in a hospice. |
| What diagnostic tests are covered? |
You will be covered in full for:
|
You will not be covered for any diagnostic tests that are:
|
| Will I be covered for surgery? |
You will be covered in full for surgery to diagnose your cancer as well as surgery to remove a primary or secondary cancer. You will also be covered for reconstructive surgery following removal of a tumour. |
You will not be covered for surgery that is unproven or experimental and not based on established medical care within the UK. |
| Will I be covered for preventative treatment? |
If you are being treated for cancer we may pay for medically necessary genetically-based tests to evaluate future risk of developing further cancers, as well as the resulting prophylactic surgery if it is recommended by your specialist. For example, we will pay for a mastectomy to a healthy breast in the event that you have been diagnosed with cancer in the other breast and your specialist indicates that prophylactic surgery is medically necessary and will be carried at the same time as surgery to the diseased breast. You must have our written agreement before you have tests, procedures or treatment and we will need full clinical details from your consultant before we can give our decision. |
|
| What drug therapies will I be covered for? |
We will pay for eligible chemotherapy and biological therapies for a maximum of 12 months or the period of the drug license, whichever is shorter. This 12 month limit will apply to primary and secondary cancers and whether is it for active or maintenance treatment. Except for cover described above, there is no cover for drug treatments given to prevent a recurrence of cancer, for the maintenance of remission or where their use is continuing without a clear end date. We will notify you in writing if cover is no longer available and assist you with making alternative arrangements where possible. |
You will not be covered for:
|
| Will I be covered for radiotherapy? |
You will be covered in full for radiotherapy, including when given for pain relief. |
|
| Will I be covered for end of life care? |
No. |
You will not be covered for treatment given solely to relieve symptoms at the end stage of cancer or treatment received in a hospice. |
| What cover will be available for routine monitoring when treatment has finished? |
You will be covered for medically necessary follow-up tests and specialist consultations needed to monitor your condition. No time limit is placed on follow-up care for cancer, as long as it is medically necessary and we receive written confirmation of this from your specialist. |
|
|
What other benefits and services are available? |
You will also be covered for:
Please see the cancer treatment benefits section in your table of benefits for full details on the additional benefits provided. |
You will not be covered for:
|
|
Are there any other limits on cover? |
|
You will not be covered for:
|
|
Are there any other supportive benefits available? |
You also have access to a comprehensive support platform delivered by Perci Health to provide you with additional support for the psychological, physical and practical impacts of cancer when it is needed most. For further information please see the your cancer support explained page. |
|
Cancer support explained
We know that a cancer diagnosis can be a life changing event and we are committed to supporting you in the event that you are impacted by cancer. This is why we have partnered with Perci Health to provide you with additional support for the psychological, physical and practical impacts of cancer.
Perci are able to offer you support regardless of how you have been impacted by cancer
- are you receiving active treatment for a cancer diagnosis?
- are you looking for some additional support following completion of your cancer treatment?
- are you caring for a loved one with cancer?
Regardless of your situation, Perci are able to provide a personalised care plan, a dedicated cancer nurse, and access to caring cancer experts from over 20 different support types to help reduce the impact of cancer.
| Recovery and rehabilitation | Symptom management | Support for carers |
|
|
|
Access to this service will not be subject to an excess, scheme underwriting or any healthcare scheme benefit limits, if any apply.
Please note; this benefit is available to members over the age of 18.
For further information and to get started access the ‘your cancer support’ tile on the Member Zone or the My Healix app.
Second medical opinion
Should you decide that you would like to receive a second medical opinion to ensure you are fully confident with your specialists recommendations please contact the claims helpline to discuss pre-authorisation. Our experienced claims team will be able to advise and support you through this process.
Second medical opinions will be arranged with a specialist who is an expert in their field and is recognised for the purposes of providing such second opinions. Without written authorisation for a second opinion, payment cannot be made for any recommended or resulting treatment.
Virtual GP
As part of your scheme you have access to a virtual GP service, called YourHealth247, which is provided by Teladoc.
You can register for this service via their portal, which can be found at:
http://www.yourhealth247.co.uk/
The portal is the fastest and easiest way to register for the virtual GP service and book your consultations. If you do not have access to the portal, you can also call YourHealth247 on 0204 586 5324.
To register, you will need your member number. This can be found on your welcome or renewal email.
Should YourHealth247 refer you onto a specialist, please contact the claims helpline to check if this is eligible under your scheme. Any onward referrals are subject to your scheme underwriting and personal exclusions (if applicable) and general scheme exclusions. Should further information on your past medical history be required, we will need your consent to contact your NHS GP.
Section 9: Glossary
The words and phrases below have the following meanings. They will appear in bold in this guide.
Active treatment
Acute condition
Annual renewal date
Benefit
Benefits
Biological therapies
Cancer
Chronic condition
Complementary practitioner
- Acupuncture practitioners must be registered with the BMAS (British Medical Acupuncture Society), BacC (British Acupuncture Council), AACP (Acupuncture Association of Chartered Physiotherapists) or AAC (The Association of Acupuncture Clinicians)
- Osteopaths must be registered with the GOsC (General Osteopathic Council)
- Chiropractors must be registered with the GCC (General Chiropractic Council) <
Daycase
Dependant
-a member’s unmarried dependent children
Dependants
-a member’s unmarried dependent children
Dialysis
- haemodialysis, (through the use of a kidney machine or dialyser)
- peritoneal dialysis (by introducing fluid into the abdomen to act as a filter). <
Disorder
Emergency
Employer
End of life care
Gender Dysphoria
Gender Incongruence
General Practitioner
GP
High dependency unit
High risk activities
Home healthcare
Hospital
Private hospital - an independent hospital which can provide acute medical, surgical or psychiatric care. It must be registered under The Registered Homes Act (1984) and approved by the Healthcare Commission or any future law. It may also include a private bed in an NHS hospital.
Inpatient
Intensive care unit
Medical condition
Medically necessary
-
In accordance with professional standards of medical practice in the United Kingdom
-
Clinically appropriate, in terms of type, frequency, extent, site and duration of treatment
-
Required for reasons other than the comfort or convenience of the patient or specialist.
-
Provided at an appropriate facility, in an appropriate setting and at an appropriate level of care for the treatment of the patient’s medical condition.
-
Provided only for an appropriate duration of time.
-
No more costly than an alternative treatment at least as likely to produce the same therapeutic or diagnostic results.
<
Members
Mental health condition
Outpatient
Palliative care
Partner
Physiotherapist
Pre-existing condition
-
you have received medication, advice or treatment, or
-
you have experienced symptoms whether the condition was diagnosed or not.
<
Private ambulance
Prosthesis
Psychological therapist
-
a psychologist who is:
-
Registered with the Health and Care Professions Council (HCPC);
-
Registered with the British Psychological Society (BPS) as a chartered Psychologist
-
a therapist who is:
-
An accredited member of the British Association of Counselling and Psychotherapy (BACP); or
-
An Accredited Member of the British Association for Behavioural and Cognitive Psychotherapies (BABCP); or
-
An Accredited Member of Scotland’s Professional Body for Counselling and Psychotherapy (COSCA); or
-
A practitioner who is registered with the United Kingdom Council for Psychotherapy (UKCP)
Registered nurse
Related condition
Specialist
- a medical practitioner with full current registration with the General Medical Council or
-
a dentist with full current registration with the General Dental Council
and
-
a specialist in the treatment you are referred for (this is applicable to all specialities including anaesthetics and psychiatry)
-
has a certificate of Higher Specialist Training in their specialty that is issued by the Higher Specialist Training Committee of the appropriate Royal College or Faculty
-
is or has been a National Health Service consultant or dentist
-
has been recognised for benefit purposes as a specialist by Healix.
<
Start date
Surgical appliance
The Scheme
Practitioner
- an occupational therapist
- an orthoptist
- a speech and language therapist
- a dietician or;
- a nurse who is on the register of the Nursing and Midwifery Council (NMC) and holds a valid NMC personal identification number. <
Treatment
Treatments
Trust Deed
Trustee, Trustees
United Kingdom
Waiting Period
We, Us, Our
You, Your
Scheme
Pandemic
Epidemic
Member Zone
Member
Neurodevelopmental disorders
Women's health services
At Healix, we know it’s vital to receive quick access to healthcare, we have therefore made access to women’s health services as easy and smooth as possible. Whenever you are experiencing a women’s health concern, you can consult with a GP with additional training in women’s health, via the virtual GP service. To access this benefit, please see the virtual GP page.
Alternatively contact the claims helpline, and speak to our experienced claims team, they will be able to guide you to the most appropriate services, including access to a remote advice service from our in-network experts.
The majority of women’s health conditions would be covered under your normal outpatient and inpatient benefits, however some conditions would traditionally sit outside the healthcare scheme cover. We have therefore created the additional women’s health benefits, to provide some extra cover, if this is required. Our experienced claims team will be able to advise you further on whether your condition and treatment would be covered under these extra benefits.
The below table outlines the services available, and how to access them through your healthcare scheme.
| Women’s health concern | How to access treatment |
|
For advice regarding any general women’s health query, including, but not limited to, menopause symptoms or contraception advice |
Access YourHealth247 through the portal to speak with a GP without contacting the claims helpline. All of the GPs are able to offer advice for common concerns, however, if you prefer you may request a consultation with a GP who specialises in women’s health. Additionally, you may self-refer by contacting the claims helpline, without the need for a GP referral, and we will be able to direct you to the most appropriate service available to you. This includes access to remote consultations and diagnostic tests, with our in-network experts (where appropriate). Cover is available up to the limits specified in your table of benefits. Once this benefit limit has been reached, the scheme rules apply as detailed in your exclusions and limitations. |
|
If you are concerned about a breast abnormality, for example a lump |
Contact the claims helpline to speak to our experienced claims team, who will be able to support you and direct you to the most appropriate specialist, without the need to see your GP first. Cover will be available as specified in your table of benefits. Further information about early signs of cancers and self-referral can be found here. |
|
If your GP has referred you to a specialist gynaecologist, for example, for unusual bleeding |
Contact the claims helpline to speak to our experienced claims team, who will be able to open a new claim. The claims team will also be able to direct you to the most suitable specialist. Cover will be available as specified in your table of benefits. |
|
If you are experiencing complications of pregnancy |
Contact the claims helpline to speak to our experienced claims team, who will be able to advise if there is any cover available for you. Cover is provided for specific pregnancy complications only, as outlined in your exclusions and limitations. |
|
For physiotherapy treatment for a pelvic problem such as stress incontinence |
Contact the claims helpline, without the need for a GP referral, and speak to our experienced claims team who will arrange a telephone based assessment with a senior physiotherapist, to determine the most appropriate treatment for you. Cover is available from your physiotherapy benefit, as specified in your table of benefits. |
Men's health services
At Healix, we know it’s vital to receive quick access to healthcare, we have therefore made access to men’s health services as easy and smooth as possible. Whenever you are experiencing a men’s health concern, you can consult with a GP with additional training in men’s health, via the virtual GP service. To access this benefit, please see the virtual GP page.
Alternatively contact the claims helpline, and speak to our experienced claims team, they will be able to guide you to the most appropriate services, including access to a remote advice service from our in-network experts.
The majority of men’s health conditions would be covered under your normal outpatient and inpatient benefits, however some conditions would traditionally sit outside the healthcare scheme cover. We have therefore created the additional men’s health benefits, to provide some extra cover, if this is required. Our experienced claims team will be able to advise you further on whether your condition and treatment would be covered under these extra benefits.
The below table outlines the services available, and how to access them through your healthcare scheme.
| Men’s health concern | How to access treatment |
|
For advice regarding any general men’s health query, including urinary symptoms, sexual health and fertility advice |
Access YourHealth247 through the portal to speak with a GP without contacting the claims helpline. All of the GPs are able to help you with common concerns. Additionally, you may self-refer by contacting the claims helpline without the need for a GP referral and we will be able to direct you to the most appropriate services available to you. This includes access to remote consultations and diagnostic tests with our in-network experts (where appropriate). Cover is available up to the limits specified in your table of benefits. Once this benefit limit has been reached the scheme rules apply as detailed in your exclusions and limitations. |
|
If you are concerned about early signs of prostate or testicular cancer |
Contact the claims helpline to speak to our experienced claims team who will be able to support you and direct you to the most appropriate specialist without the need for seeing your GP first. Cover will be available as specified in your table of benefits. Further information about early signs of cancers and self-referral can be found here. |
|
If your GP has referred you to a specialist |
Contact the claims helpline or access the claims portal to open a new claim. Cover will be available as specified in your table of benefits. One of our experienced claims team will be able to direct you to the most suitable specialist. |
|
For physiotherapy treatment for a pelvic problem such as stress incontinence |
Contact the claims helpline, without the need for a GP referral, and speak to our experienced claims team who will arrange a telephone based assessment with a senior physiotherapist, to determine the most appropriate treatment for you. Cover is available from your physiotherapy benefit, as specified in your table of benefits. |
Self-referred cancer benefits
Experiencing symptoms that can be associated with cancer can be concerning. It's important to remember that these symptoms are not definitive of cancer but may indicate a risk. We are here to support you in obtaining timely investigations for any symptoms that could potentially be related to cancer.
If you experience any of the symptoms listed below then you are able to call and speak directly to our experienced claims team to self-refer for a consultation and diagnostic tests.
This means that you no longer need to see your GP before accessing private treatment for these concerns in order to prevent any delays in reaching a diagnosis.
If you are experiencing any of the symptoms below, contact the claims helpline and our experienced claims team will be able to help direct you into one of our robust clinical pathways with our in-network providers to help reach a diagnosis.
| Type of cancer | Signs and symptoms to watch out for |
|
Breast cancer |
|
|
Bowel cancer |
|
|
Prostate cancer |
Raised PSA level as specified below:
|
|
Testicular cancer |
|
|
Skin cancer |
Any of the following changes to a mole or lesion on the skin:
|
Please remember that these signs are also features of common health problems that
are not caused by cancer, such as a cyst, piles or infection.
In the event that a cancer diagnosis is made, cover will be available as detailed in your cancer cover explained and one of our nurse case managers will support you and be able to provide information on the treatment options available to you.
Please contact us via the Member Zone, the My Healix app or the claims helpline to get further advice and to open a new claim. As with all of your healthcare benefits it is important that you obtain pre-authorisation before receiving any treatment to ensure your claim is eligible and to prevent you incurring any unwanted costs.
Musculoskeletal health pathway
Musculoskeletal conditions affect your muscles, bones and joints. They are very common and tend to increase with age.
Pain and discomfort can affect your daily activities but early diagnosis and treatment may help to ease your symptoms and improve the length of time it takes to recover. We have designed the Healix musculoskeletal pathway with this in mind.
How to make a claim
As soon as you experience bone or joint pain you can use our digital physiotherapy triage service. The service is available for everyone over the age of 16.
This can be accessed via the Member Zone or the My Healix app where you will be directed straight through to begin your online journey and treatment pathway without the need to contact the claims helpline.
Access the Member Zone
Click here to access the Member Zone using your individual member number
This digital service is designed to provide an assessment of your needs and guide you to the best course of treatment.
Where self-managed care is appropriate, you are able to immediately access a tailored exercise programme with in-app access to a clinician as required. If needed, you will be guided to face-to-face physiotherapy treatment with our network provider.
If face-to-face physiotherapy sessions are recommended these will not be subject to an excess, scheme underwriting or any scheme limits (if these apply) when treatment is taken with our digital treatment pathway provider. All other healthcare scheme terms and conditions will apply.
Telephone assessment
If you are unable to access the Member Zone or the My Healix app, contact the claims helpline to arrange a telephone based clinical assessment. Our experienced claims team will take your details and arrange for you to have an initial telephone consultation with a physiotherapist at a convenient time for you who will recommend the most appropriate treatment.
The telephone-based clinical assessment will not be subject to any excess, if one applies, however it will be applied to face-to-face treatment should this be required. All other healthcare scheme terms and conditions will apply.
Mental health pathway
The importance of mental health and wellbeing is becoming increasingly recognised in today’s busy world. Acknowledging stress and anxiety then seeking help are the first steps to developing coping strategies and recovery.
If you are experiencing stress, anxiety or depression or any other mental health problem, please refer to the below for further information on how your scheme can support you
How to make a claim
Members are able to access a digital emotional wellness triage and immediate advice via the Member Zone or the My Healix app. The service is available for everyone over the age of 16.
Access the Member Zone
Click here to access the Member Zone using your individual member number
| Benefits | What is available? | What can you use this for? |
| Digital emotional wellness triage |
|
|
If face-to-face mental health treatment is recommended you will be directed to your GP / primary care service to access this via the NHS.
Digital skin pathway
Changes found to your skin can be concerning. Fortunately, in most instances, these changes are not caused by cancer, however fast detection is key to help identify the cause of these changes and provide reassurance.
Our digital skin pathway provides fast results and recommendations for further treatment depending on your diagnosis following assessment by our dermatology partners. Please note further treatment will be subject to the terms and conditions of the scheme.
This pathway is suitable for many skin complaints, and our experienced claims team will be able to guide you to access the most suitable pathway for your symptoms.
The table below shows which skin complaints are most suitable to be referred into our digital skin pathway:
| Skin conditions suitable for the skin pathway | Skin conditions not suitable for the skin pathway |
|
|
How to access the digital skin pathway
Our digital skin pathway is designed to be simple and efficient. Follow the steps below to access fast, expert care:
Please note, face-to-face consultations with dermatologists within our network will not be subject to our reasonable and customary fees. If you choose to consult outside our network, these guidelines will apply.
Section 9: Glossary
The words and phrases below have the following meanings. They will appear in bold in this guide.
Active treatment
Acute condition
Annual renewal date
Benefit
Benefits
Biological therapies
Cancer
Chronic condition
Complementary practitioner
- Acupuncture practitioners must be registered with the BMAS (British Medical Acupuncture Society), BacC (British Acupuncture Council), AACP (Acupuncture Association of Chartered Physiotherapists) or AAC (The Association of Acupuncture Clinicians)
- Osteopaths must be registered with the GOsC (General Osteopathic Council)
- Chiropractors must be registered with the GCC (General Chiropractic Council) <
Daycase
Dependant
-a member’s unmarried dependent children
Dependants
-a member’s unmarried dependent children
Dialysis
- haemodialysis, (through the use of a kidney machine or dialyser)
- peritoneal dialysis (by introducing fluid into the abdomen to act as a filter). <
Disorder
Emergency
Employer
End of life care
Gender Dysphoria
Gender Incongruence
General Practitioner
GP
High dependency unit
High risk activities
Home healthcare
Hospital
Private hospital - an independent hospital which can provide acute medical, surgical or psychiatric care. It must be registered under The Registered Homes Act (1984) and approved by the Healthcare Commission or any future law. It may also include a private bed in an NHS hospital.
Inpatient
Intensive care unit
Medical condition
Medically necessary
-
In accordance with professional standards of medical practice in the United Kingdom
-
Clinically appropriate, in terms of type, frequency, extent, site and duration of treatment
-
Required for reasons other than the comfort or convenience of the patient or specialist.
-
Provided at an appropriate facility, in an appropriate setting and at an appropriate level of care for the treatment of the patient’s medical condition.
-
Provided only for an appropriate duration of time.
-
No more costly than an alternative treatment at least as likely to produce the same therapeutic or diagnostic results.
<
Members
Mental health condition
Outpatient
Palliative care
Partner
Physiotherapist
Pre-existing condition
-
you have received medication, advice or treatment, or
-
you have experienced symptoms whether the condition was diagnosed or not.
<
Private ambulance
Prosthesis
Psychological therapist
-
a psychologist who is:
-
Registered with the Health and Care Professions Council (HCPC);
-
Registered with the British Psychological Society (BPS) as a chartered Psychologist
-
a therapist who is:
-
An accredited member of the British Association of Counselling and Psychotherapy (BACP); or
-
An Accredited Member of the British Association for Behavioural and Cognitive Psychotherapies (BABCP); or
-
An Accredited Member of Scotland’s Professional Body for Counselling and Psychotherapy (COSCA); or
-
A practitioner who is registered with the United Kingdom Council for Psychotherapy (UKCP)
Registered nurse
Related condition
Specialist
- a medical practitioner with full current registration with the General Medical Council or
-
a dentist with full current registration with the General Dental Council
and
-
a specialist in the treatment you are referred for (this is applicable to all specialities including anaesthetics and psychiatry)
-
has a certificate of Higher Specialist Training in their specialty that is issued by the Higher Specialist Training Committee of the appropriate Royal College or Faculty
-
is or has been a National Health Service consultant or dentist
-
has been recognised for benefit purposes as a specialist by Healix.
<
Start date
Surgical appliance
The Scheme
Practitioner
- an occupational therapist
- an orthoptist
- a speech and language therapist
- a dietician or;
- a nurse who is on the register of the Nursing and Midwifery Council (NMC) and holds a valid NMC personal identification number. <
Treatment
Treatments
Trust Deed
Trustee, Trustees
United Kingdom
Waiting Period
We, Us, Our
You, Your
Scheme
Pandemic
Epidemic
Member Zone
Member
Neurodevelopmental disorders
Making a claim
Register your claim using our My Healix app or Member Zone. Alternatively, you can contact the claims helpline to confirm if cover is available.
In order for us to accurately assess cover under the terms and conditions of your scheme, we may ask to see a copy of your GP referral letter when you open a new claim.
Always contact the claims team before arranging or receiving any treatment.
Access the Member Zone
Click here to access the Member Zone using your individual member number
Contact the claims helpline:
0208 763 3405
Monday-Friday 08.00-19.00 (Excl. bank holidays)
Saturday 09.00-13.00
We will confirm:
-
whether your proposed treatment is eligible for cover under the scheme
-
whether your proposed treatment costs will be covered under the scheme
-
any benefit limits or excess that may apply to your claim
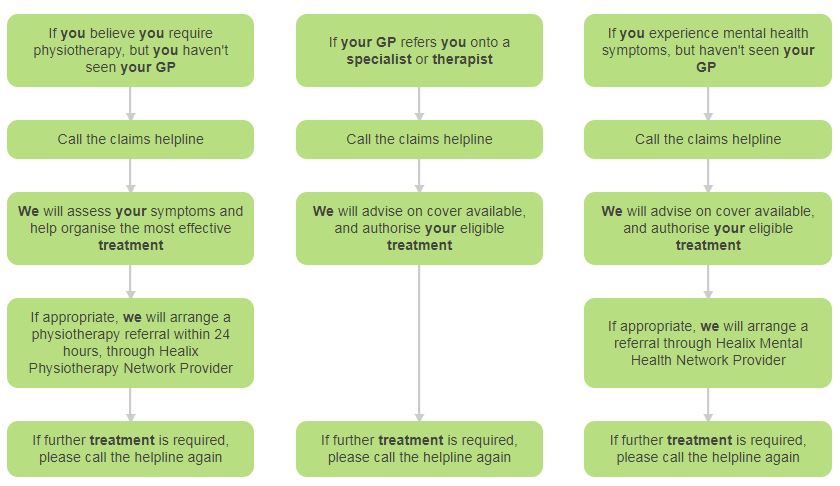
To help you make the best possible use of the scheme, we have provided you with a how to claim summary.
How to claim summary
If you believe you require physiotherapy, but you haven't seen your GP
If your GP refers you onto a specialist or therapist
If you experience mental health symptoms, but haven't seen your GP
Log your claim via the Member Zone, the My Healix app or contact the claims helpline
Log your claim via the Member Zone, the My Healix app or contact the claims helpline
Log your claim via the Member Zone, the My Healix app or contact the claims helpline
We will assess your symptoms and help organise the most effective treatment
We will advise on cover available, and authorise your eligible treatment
We will advise on cover available, and authorise your eligible treatment
If appropriate, we will arrange a physiotherapy referral within 24 hours, through Healix Physiotherapy Network Provider
If appropriate, we will arrange a referral through Healix Mental Health Network Provider
If further treatment is required, please visit the Member Zone, the My Healix app or contact the claims helpline again
If further treatment is required, please visit the Member Zone, the My Healix app or contact the claims helpline again
If further treatment is required, please visit the Member Zone, the My Healix app or contact the claims helpline again
Your scheme underwriting
Medical History Disregarded (MHD)
We will not apply any personal medical exclusions to your scheme. However your eligibility for cover will be subject to the general terms of the scheme. Please refer to your exclusions and limitations for further information.
Reasonable and customary fees
We adhere to a schedule of reasonable and customary (R&C) fees for specialist fees. These are based on a common set of codes and principles set out by the Clinical Classification and Schedule Development (CCSD) group. Our fee levels have been set after review of what the majority of specialist’s charge for medical and surgical services as well as a review by our clinical support team and our panel of specialist advisors.
We have an open referral network which means you can be referred to the specialist of your choice. Should you choose to be referred to a specialist who charges above our fee schedule you can opt to pay the difference or we can assist you in identifying an alternative specialist that charges within our fee schedule. For further information please refer to our fee schedule, or contact the claims helpline.
Your excess
All members and dependants are liable for an excess of £100, which is payable once every scheme year, if you make an eligible claim.
Your excess will be applied to the first eligible treatment that you receive in each scheme year. This is regardless of when the last excess payment was made and whether the treatment is for the same condition, a related condition, or for an entirely new condition. Please contact the claims helpline before you receive any treatment, so that we can advise you on when your excess will apply.
What happens in an emergency?
Most private hospitals are not set up to receive emergency admissions. In the event of an emergency you should:
- call for an NHS ambulance
- visit the accident and emergency department at the local NHS hospital.
If you would like to be transferred to a private facility, please contact the claims helpline to discuss this. We will then be able to confirm whether your proposed treatment is eligible under the healthcare scheme. Please note you must contact us before you transfer to a private facility.
You will not be covered for:
- the cost of emergency treatment in a private walk-in centre, accident and emergency department or clinic
- the cost of treatment in an intensive care or high dependency unit if you have been transferred specifically to receive this care
- the costs of the transfer to a private facility specifically to receive treatment in an intensive care or high dependency unit.
Exclusions and limitations
The following are conditions and treatments which are not covered under your scheme. If you are unsure about anything in this section, please contact the claims helpline.
We do not pay for treatment to relieve symptoms commonly associated with or caused by ageing, puberty or other natural physiological cause.
Please note: we will pay for remote consultations and diagnostics with our in-network experts in women’s or men's health, as specified in your table of benefits.
We do not pay for any treatment required for alcohol, solvent or drug abuse, or any treatment arising from such abuse or addiction.
We do not pay for the supply or fitting of appliances, physical aids or devices (including but not limited to hearing aids, spectacles, contact lenses, crutches, walking sticks external prostheses and orthotics etc) which do not fall within our definition of surgical appliance. Any consultations relating to these are also not covered.
Please note: we will pay for medically necessary orthotics as detailed in your table of benefits.
We do not pay for artificial life maintenance (including mechanical ventilation) where such treatment will not or is not expected to result in your recovery or restore you to your previous state of health.
We do not pay for:
- birth control
- sterilisation and/or reversal
- termination of pregnancy
Please note: we will pay for remote consultations and diagnostics with our in-network experts in women’s or men's health, as specified in your table of benefits.
We do not pay for treatment of chronic conditions. By this we mean any medical condition which has at least one of the following characteristics:
- it needs ongoing or long-term monitoring through consultations, examinations, check-ups and/or tests
- it needs ongoing or long-term control or relief of symptoms
- it requires rehabilitation or for you to be specially trained to cope with it
- it continues indefinitely
- it has no known cure
- it comes back or is likely to come back
Please note: this will apply to all medical conditions, whether or not a diagnosis has been made.
Exception: we will pay for eligible treatment arising out of a chronic condition, or for treatment of acute symptoms of a chronic condition that flare up. However, we only pay if the treatment is likely to lead quickly to a complete recovery or to you being fully restored to your previous state of health, without you having to receive prolonged treatment. For example, we pay for treatment following a heart attack arising out of chronic heart disease. This exception does not apply to treatment of a mental health condition.
Please note: in some cases it might not be clear, at the time of treatment, that the disease, illness or injury being treated is a chronic condition. We are not obliged to pay the ongoing costs of continuing, or similar, treatment. This is the case even where we have previously paid for this type of or similar treatment.
Please note this exclusion does not apply to the treatment of cancer.
Please note there is some cover for chronic conditions. Please refer to your table of benefits for further information.
We do not pay for treatment which arises from, or is related to any exclusion listed in this scheme handbook or treatment which arises from or is related to a surgical procedure we do not cover.
We do not pay any treatment costs, including any increased treatment costs, you incur because of complications caused by a disease, illness, injury or treatment for which benefit has been excluded or restricted under your benefits.
We do not pay for treatment of any disease, illness, injury or disability which is caused or contributed to by; nuclear, radioactive, biological or chemical contamination, war (whether declared or not), act of foreign enemy, riot, revolution, invasion, civil war, rebellion, insurrection, overthrow of a legally constituted government, explosions of war weapons, terrorist act or military activity. We will not pay for treatment of any disease, illness, injury or disability which is received while you or your dependants are carrying out army, naval or air services duties.
We do not pay for treatment if it is primarily used for domestic and/or social reasons.
Exception: we will pay up to 28 days of inpatient, daycase and/or outpatient rehabilitation treatment which is intended to restore health or mobility with the aim of returning you to independent living. The rehabilitation must be referred by a specialist and be an integral part of eligible treatment. Treatment must take place within 12 months of you having been deemed medically fit to commence rehabilitation by your specialist.
We do not pay for any treatment to change your appearance even when required for psychological reasons.
We do not pay for any treatment, including surgery:
- where the intention of treatment, whether directly or indirectly, is the reduction or removal of healthy, surplus or fat tissue (for example, weight reduction surgery / treatment)
- where the aim is to aesthetically enhance the appearance of the face or body where no functional condition is present (for example, botox, fillers or asymptomatic rhinoplasty)
Exception: we will pay for medically necessary treatment to restore your appearance in the following circumstances:
- where it results from an eligible underlying disease process
- following eligible treatment (including cancer treatment)
- where the condition is causing a functional problem
Please note: we use clinical guidance as a benchmark for deciding whether the exceptions above are eligible for cover. All requests for cover must be submitted in writing with supporting medical information.
We do not pay for treatment for or arising from deafness caused by a congenital abnormality, maturing or ageing.
Exception: we will pay for treatment for hearing impairment or deafness that arises as a result of an acute condition diagnosed within the previous 12 months. For example, glue ear or perforated eardrum.
We do not pay for any dental or oral treatment other than as listed in the exception below.
Exception: we will pay for eligible treatment related only to the following specified oral surgical operations when carried out by a specialist:
- surgically remove a complicated, buried, infected or impacted tooth root
- apicectomy or removal of the tip of a tooth’s root
- enucleation of a cyst of the jaw (removing a cyst from the jaw bone)
- surgical drainage of a fascial space (tracking) abscess
- putting a natural tooth back into a jaw bone after it is knocked out or dislodged in an accident
- treatment of facial and mandibular fractures.
We do not pay for treatment for or associated with dialysis, unless it is required as a complication in the short term following eligible treatment.
We do not pay for drugs and dressings provided or prescribed for use as an outpatient or for you to take home other than those outlined in your cancer cover explained.
We do not pay for:
- the cost of emergency treatment in a private walk-in centre, accident and emergency department or clinic
- the cost of an emergency admission into a private hospital
- the cost of treatment in an intensive care or high dependency unit if you have been transferred specifically to receive this care
- the costs of the transfer to a private facility specifically to receive treatment in an intensive care or high dependency unit.
We do not pay for treatment when you are near or approaching the end of life and active treatment for the causative disease is no longer considered effective or appropriate.
We do not pay for treatments including medication, which in our reasonable opinion are experimental or not yet approved by the National Institute for Clinical Excellence, are being researched or that do not yet have sufficient peer-reviewed evidence to conclude that:
- the harmful effects are outweighed by the beneficial effects
- they are likely to lead to the same or better outcomes than available alternatives
- they are based on established medical practice in the United Kingdom
We will evaluate therapy not yet considered by NICE on a case by case basis using all currently available evidence from properly controlled mature phase III clinical trials and may pay for the use of a new, licensed anti-cancer drug, or new use for a drug with a licensed indication where there is credible scientific evidence to support its use.
We do not pay any treatment costs you incur because of any complications arising or resulting from experimental treatment that you receive or for any subsequent treatment you may need as a result of you undergoing any experimental treatment.
We do not pay for treatment to correct your eyesight due to long or short vision, including but not limited to, laser eye surgery, spectacles or contact lenses.
Please note: we will pay for eligible treatment to the eye resulting from an acute condition or injury.
We do not pay for:
- any type of fertility investigations
- fertility treatment
- assisted reproduction, surrogacy, harvesting of donor eggs or donor insemination
- sperm collection and storage
- complications following any of the above
Please note: we will pay for remote consultations and diagnostics with our in-network experts in women’s or men's health, as specified in your table of benefits.
We do not pay for any treatment of gender dysphoria, or any treatment arising from or relating to gender dysphoria.
We do not pay for any GP consultations or visits other than those specified in your table of benefits. We do not pay for any charges for the completion of claim forms or referral letters, unless we have requested these specifically to assess your claim.
We do not pay for treatment or charges incurred in nature cure clinics, health hydros, spas or similar establishments is not covered, even if they are registered as, or part of a listed hospital, including private beds registered as a nursing home in these places.
We do not pay for hormone Replacement Therapy (HRT) or bone densitometry is not covered.
Exceptions:
- we will pay for bone densitometry if it is recommended by your specialist to help determine or assess your condition as part of eligible treatment which we have agreed in writing and in advance. We will require full clinical details from your specialist
- we will pay for Hormone Replacement Therapy if it is medically indicated as a result of medical intervention. We will only pay for specialist consultations and for the cost of implants. We will not cover the cost of patches or tablets. Benefit will only be paid for a maximum of 18 months from the date of medical intervention.
We do not pay for charges incurred in a private hospital or any NHS hospital for ITU (Intensive Therapy Unit) or ICU (Intensive Care Unit) treatment, unless the treatment immediately follows and is required as a result of eligible pre-authorised treatment for which we have provided written confirmation that benefits will be payable.
We do not pay for treatment of or monitoring and investigations into any mental health, emotional or behavioural condition or illness, whether or not this is under the direct control of a Consultant Psychiatrist, this includes eating disorders.
We do not pay for any treatment (including assessment) of adult or childhood neurodevelopmental disorders.
We do not pay for any weight loss treatment or treatment required as a result of obesity.
We do not pay for treatment outside the United Kingdom including evacuation or repatriation, other than as specified in your table of benefits.
We do not pay for treatment for or arising from pandemic and/or epidemic disease.
We do not pay for personal comfort and convenience items or services such as television, telephone costs, newspapers, taxi fares, guest meals and similar incidental services and supplies.
We do not pay for any treatment related to pregnancy or childbirth, other than as listed in the exception below:
Exception: we will pay for the following eligible specified obstetric procedures / treatment:
- pelvic girdle pain in pregnancy
- miscarriage or when the foetus has died and remains with the placenta in the womb
- still birth
- hydatidiform mole (abnormal cell growth in the womb)
- ectopic pregnancy (foetus growing outside the womb)
- diastasis recti or Rectus Abdominis (splitting of the abdominal muscles during pregnancy)
- post-partum haemorrhage (heavy bleeding in the hours and days immediately after childbirth)
- retained placental membrane (afterbirth left in the womb after the delivery of the baby)
- eligible mental health treatment for post-natal depression subject to the conditions and limitations set out in the mental health benefit
- medically essential caesarean section where this is an inevitable consequence of a complication to the current pregnancy
- complications following any of the above conditions
- flare up of a non-pregnancy related medical condition that has been made worse by pregnancy
We will require full clinical details from your specialist before we can give our decision on cover.
In the event that the newborn requires immediate treatment as a result of an eligible caesarean section, this should be administered by the NHS free of charge. If the newborn is not entitled to NHS care and is not accepted as a dependant on the scheme we will pay for treatment for up to 7 days following the birth, to allow you time to make alternative arrangements. In cases where they are accepted as a member of the scheme they will only be entitled to benefits outlined in the benefits table and will be subject to the exclusions listed within the scheme.
We do not pay for treatment required as a consequence of injury sustained whist training for, or participating in, sport for which you receive payment or sponsorship (other than travel costs).
We do not pay for any form of genetic testing or screening, health screening, health checks or preventative treatment, procedures or medical services where no disease is present.
We do not pay for treatment;
- recommended because of a genetic predisposition towards developing a medical condition
- recommended because of a family history of a medical condition.
We do not pay for:
- any treatment required directly or indirectly as a result of self-inflicted illness, or injury, or suicide attempt
- any treatment directly or indirectly arising from participation in professional, hazardous or dangerous sports, unless such participation was disclosed to and accepted by us in writing
- any treatment resulting from an injury sustained in an accident for which you may be or have been subject to criminal proceedings
- any treatment resulting from a road accident where you were not wearing a seat belt as required by law.
- any treatment resulting from high-risk activities such as mountaineering, rock climbing, parachuting, hang-gliding, potholing, bungee jumping, racing of any kind, skiing or snowboarding off the designated course (off-piste), scuba diving (unless you have recognised diving qualifications or are accompanied by someone with them. This list is not exhaustive, please contact the claims helpline if you need further information).
We do not pay for any treatment required due to sexual dysfunction, sexually transmitted infections or sexual problems, whatever the cause.
Please note: we will pay for remote consultations and diagnostics with our in-network experts in women’s or men's health, as specified in your table of benefits.
We do not pay for treatment for or relating to any speech disorder such as stammering. However we may pay for short term speech therapy for an acute condition immediately following eligible treatment. The speech therapy must be recommended by a specialist in charge of treatment.
We do not pay for treatment needed for any procedure required to a mother or child as a result of a surrogate pregnancy until such time as the child has been accepted as an eligible dependant by the scheme. At which time the child only will be entitled to benefits outlined in the table of benefits.
We do not pay for treatment intended to provide temporary relief of symptoms or for the ongoing management of a condition.
We do not pay for any transplants, adoptive cell transfer, gene therapies and/or any complications related to, or resulting from these treatments. This includes, but is not limited to CAR T cell therapy, Tumour Infiltrating Lymphocyte therapy and stem cell/bone marrow treatments.
We also do not pay for:
- donor costs
- harvesting
- storage
- administration
- and/or any complications/treatment arising from any of the above
Please note: we will pay for recipient costs for skin or corneal grafts when eligible for benefit.
We do not pay for travel costs to and from medical facilities (including parking costs) for treatment.
We do not pay for treatment as a result of injuries or illness caused by you carrying out an illegal act.
We do not pay for the treatment of warts or verrucas or any related conditions.
We do not pay for any expenses which you have claimed or can claim from any other insurance or source. If another insurer provides cover, we will negotiate with them to make sure both companies pay their share of the claim.
You must tell us in writing as soon as possible about any claim or right of legal action, against any other person that arises from the claim under this scheme.
You must keep us fully informed of any developments.
If we ask you, you must take all steps to include the amount of benefit you are claiming from us under this scheme in your claim against the other person. We can take over and defend or settle any claim or prosecute any claim, in your or your dependant’s name for our own benefit.
We will decide how to carry out any proceedings and settlement.
We do not pay for any treatment that has not been referred by:
- your GP
- an optician for eye treatment
Please note: you may be able to self refer for treatment, please refer to your table of benefits for further information.
We do not pay for treatment provided by a specialist, practitioner, physiotherapist, complementary practitioner and/or supplier of services we do not recognise as being qualified to provide the type of treatment you need or for treating the medical condition you have.
We do not pay for treatment with sports therapists, massage therapists, or anyone who does not meet our definition of a practitioner or complementary practitioner.
We do not pay for any vaccinations or immunisations.
Section 9: Glossary
The words and phrases below have the following meanings. They will appear in bold in this guide.
Active treatment
Acute condition
Annual renewal date
Benefit
Benefits
Biological therapies
Cancer
Chronic condition
Complementary practitioner
- Acupuncture practitioners must be registered with the BMAS (British Medical Acupuncture Society), BacC (British Acupuncture Council), AACP (Acupuncture Association of Chartered Physiotherapists) or AAC (The Association of Acupuncture Clinicians)
- Osteopaths must be registered with the GOsC (General Osteopathic Council)
- Chiropractors must be registered with the GCC (General Chiropractic Council) <
Daycase
Dependant
-a member’s unmarried dependent children
Dependants
-a member’s unmarried dependent children
Dialysis
- haemodialysis, (through the use of a kidney machine or dialyser)
- peritoneal dialysis (by introducing fluid into the abdomen to act as a filter). <
Disorder
Emergency
Employer
End of life care
Gender Dysphoria
Gender Incongruence
General Practitioner
GP
High dependency unit
High risk activities
Home healthcare
Hospital
Private hospital - an independent hospital which can provide acute medical, surgical or psychiatric care. It must be registered under The Registered Homes Act (1984) and approved by the Healthcare Commission or any future law. It may also include a private bed in an NHS hospital.
Inpatient
Intensive care unit
Medical condition
Medically necessary
-
In accordance with professional standards of medical practice in the United Kingdom
-
Clinically appropriate, in terms of type, frequency, extent, site and duration of treatment
-
Required for reasons other than the comfort or convenience of the patient or specialist.
-
Provided at an appropriate facility, in an appropriate setting and at an appropriate level of care for the treatment of the patient’s medical condition.
-
Provided only for an appropriate duration of time.
-
No more costly than an alternative treatment at least as likely to produce the same therapeutic or diagnostic results.
<
Members
Mental health condition
Outpatient
Palliative care
Partner
Physiotherapist
Pre-existing condition
-
you have received medication, advice or treatment, or
-
you have experienced symptoms whether the condition was diagnosed or not.
<
Private ambulance
Prosthesis
Psychological therapist
-
a psychologist who is:
-
Registered with the Health and Care Professions Council (HCPC);
-
Registered with the British Psychological Society (BPS) as a chartered Psychologist
-
a therapist who is:
-
An accredited member of the British Association of Counselling and Psychotherapy (BACP); or
-
An Accredited Member of the British Association for Behavioural and Cognitive Psychotherapies (BABCP); or
-
An Accredited Member of Scotland’s Professional Body for Counselling and Psychotherapy (COSCA); or
-
A practitioner who is registered with the United Kingdom Council for Psychotherapy (UKCP)
Registered nurse
Related condition
Specialist
- a medical practitioner with full current registration with the General Medical Council or
-
a dentist with full current registration with the General Dental Council
and
-
a specialist in the treatment you are referred for (this is applicable to all specialities including anaesthetics and psychiatry)
-
has a certificate of Higher Specialist Training in their specialty that is issued by the Higher Specialist Training Committee of the appropriate Royal College or Faculty
-
is or has been a National Health Service consultant or dentist
-
has been recognised for benefit purposes as a specialist by Healix.
<
Start date
Surgical appliance
The Scheme
Practitioner
- an occupational therapist
- an orthoptist
- a speech and language therapist
- a dietician or;
- a nurse who is on the register of the Nursing and Midwifery Council (NMC) and holds a valid NMC personal identification number. <
Treatment
Treatments
Trust Deed
Trustee, Trustees
United Kingdom
Waiting Period
We, Us, Our
You, Your
Scheme
Pandemic
Epidemic
Member Zone
Member
Neurodevelopmental disorders
End of cover
Cover for you (the member) will end in the following situations:
-
if your employment with Baxter has come to an end for any reason
-
if you no longer live full time in the United Kingdom
-
if you pass away
-
if for any reason you or Baxter ask us to end cover
- If you or any of your dependants have given us misleading information, have kept something from us, or have broken the conditions of this plan.
If your cover ends, your dependants cover will also end on the same day as your cover.
Cover for dependants will end in the following situations:
Your partner's cover will end:
-
if you get divorced, or your civil partnership is dissolved. Cover for your partner will end as soon as the final decree/final dissolution order has been granted.
-
if you no longer live together, then your partner will no longer be considered a dependant for the purposes of this scheme.
Your dependant child’s cover will end:
-
after they have turned 29. They will be removed from cover on the next annual renewal date following their 29th birthday.
-
if they get married, then they will no longer be considered a dependant for the purposes of this scheme.
- if they no longer live full time in the United Kingdom
Any dependants who remain on cover past the current maximum age (renewal following 29th birthday) will be charged as a single adult on the scheme therefore if an employee is on single parent family or family cover and their dependant remains on cover past 29 then they will be charged for single cover or couple cover.
Over aged dependants may remain on cover if the dependants are:
- unmarried
- living with their parents
- still financially dependent on their parents.
Employees must inform their HR department as soon as possible of any changes of this matter.
If treatment has been authorised, but has not yet taken place, you will be responsible for any treatment costs if the scheme then terminates or you leave the scheme.
Continuation option
As Healix Health only provides corporate group schemes, we are unable to continue your cover as an individual if you leave the Baxter Healthcare Scheme.
We understand the importance of your healthcare and choosing a new provider may be daunting. We work closely with two providers to provide you with the best choice possible to take your healthcare forward.
What is a continuation option?
A continuation option allows members who resign or retire from an employer that provides workplace healthcare benefits to take out their own cover. You might be eligible to take over the benefits previously paid for by the employer, however it’s not always guaranteed that any ongoing claims will be covered.
National Friendly
Who are NF?
A Friendly Society that helps its members meet their health protection needs by offering you cover through private medical insurance policies.
How do I contact them?
Call 0333 014 6244, (8am-6pm Monday to Friday). Quote HEALIX and the team will be able to obtain the best possible terms for your transition.
What do they cover?
My Private Medical Insurance policy is a flexible product that offers cover for everyone up to age 85. You can choose between guided outpatient only cover all the way through to unlimited inpatient cover.
To find out more about National Friendly visit here.
Usay Compare
Who are Usay?
The largest individual health insurance intermediary and are experts at finding the best cover for you.
How do I contact them?
Call 01285 864670 and quote HEALIX.
What do they cover?
Usay Compare will get to know your unique individual requirements, do all the hard work comparing prices and policies for you; then advise on the best and most cost-effective quote.
To find out more about Usay Compare, fill in this online form.
These terms are offered to you as a previous member of the healthcare scheme and are available for a limited time only, usually no more than 30 days from the date of leaving. It is therefore important that you act quickly to maintain continuity of cover.
Health Services Ltd is an introducer appointed representative of both National Friendly and Usay Business Ltd, who are authorised and regulated by the Financial Conduct Authority. Calls may be recorded or monitored for quality control.
How to make a complaint
It is always our intention to provide a first class standard of service: however, we recognise that on occasions, your requirements may not have been met.
Should you have any cause for complaint, you should contact the claims helpline.
How your complaint will be handled
Stage 1
You will receive a written acknowledgement of your complaint within five business days of receipt. This will include the name and job title of the individual handling the complaint.
Stage 2
Within four weeks of receiving your complaint, you will receive either:
-
A final response or
-
A holding response, explaining why we are not yet in a position to resolve the complaint and indicating when we will be making further contact (this will be within eight weeks from receiving the complaint).
Stage 3
If you have not received a final response within four weeks, by the end of eight weeks after receipt of the complaint, you will receive either:
-
A final response.
-
A response explaining why we are still not in a position to provide a final response and explaining when we believe we will be able to do so.
-
If we are unable to provide a final response, due to the delay which has now occurred, you may refer your complaint to the Trustees.
If, during stage 2 or 3, we issue our final response but you remain dissatisfied, you may refer your complaint to the Trustees. To do this, please set out your reasons fully in writing to the Operations Director, asking for referral to the trustees for further consideration.
How to claim reimbursement
How to claim for cash benefits
If you have received eligible treatment free of charge on the NHS you may be eligible to receive reimbursement of cash benefits as detailed in your table of benefits.
These benefits will only be eligible if the treatment received would otherwise have been eligible for benefit under your scheme.
Please note; only one cash benefit reimbursement can be claimed per admission.
In order to claim these benefits you can register your claim via the Member Zone or the My Healix app.
You will need to provide the following information for a claim to be processed
- a copy of your NHS discharge paperwork which should confirm the following information:
- date of admission and discharge from the NHS hospital
- name and date of birth of the person admitted to hospital
- summary of the reason for admission and the treatment received
- bank details for the reimbursement to be made to
- account holder’s name
- sort code
- account number
How to claim reimbursement of medical expenses
If you have paid a provider directly for eligible medical services, you can claim a reimbursement of these costs as long as the treatment received is eligible for cover as detailed in your table of benefits.
In order to claim these benefits you can register your claim via the Member Zone or the My Healix app.
You will need to provide the following information for a claim to be processed:
- an itemised receipt confirming the following information:
- date treatment was received
- details of the treatment received
- amount paid for the treatment
- bank details for the reimbursement to be made to
- account holder’s name
- sort code
- account number
Please note:
Once the claim has been confirmed as eligible by our experienced claims team, reimbursement will be arranged via direct bank transfer.
All reimbursement claims (including cash benefit claims) must be submitted within six months of your treatment date / birth or adoption date.
Additional information can be found in the payment of invoices page.
Payment of invoices
It's essential that all treatment is pre-authorised. This allows us to place a guarantee of payment with your healthcare provider, subject to your benefit limits and our reasonable and customary fees. If you have pre-authorised your treatment, we will settle the bill (up to applicable limits) directly with your specialist, therapist or hospital. You are responsible for making sure we have all the information we need to pay your claims.
In some circumstances it may be necessary for you to pay for pre-authorised treatment yourself, and request a reimbursement from us for the cost of the treatment. In these cases please submit a copy of your receipt via Member Zone or the My Healix App, along with your bank account details, and we will arrange reimbursement via direct bank transfer. All reimbursement claims (including cash benefit claims) must be submitted within six months of your treatment date.
We will not pay for claims if:
- the invoice or reimbursement claim (including cash benefit claims) is not submitted within six months of your treatment date
- if the treatment takes place after you have left the scheme
- if you break any terms and conditions of your membership
- if you incur a fee for non-attendance or late cancellations
Requests for additional information
We may ask you to provide information to help us assess your claim. For example we may ask you for one or more of the following:
-
medical reports and other information about the treatment for which you are claiming. If we request a medical report from your specialist and they charge for providing this we will pay the cost
-
original accounts and invoices in connection with your claim
-
obtain results of an independent medical examination or second opinion for which we may ask you to make an appointment with a with a specialist. We will pay for the cost of any independent medical examination or second opinion we require and we will authorise this in writing, in advance
-
provide results of any second opinion you have independently sought under the care of another specialist. On such occasions we may additionally request our own, independent, second opinion from an expert in that field to assess eligibility of cover. We will pay the costs of any second opinion we organise on your behalf, this includes the cost of the consultation and any tests undertaken as a result of that consultation
We will liaise with you and your medical specialists throughout your treatment and will request medical information, when we deem this to be necessary for the assessment of your claim. You will be asked for your consent before we do this.
Throughout your claim we will make you aware of the options that are available to you. If your medical specialist recommends treatment, you should contact the claims helpline as soon as possible to be sure that continued treatment is covered.
Our experienced claims team will assess the level of cover available to you for planned treatment within the terms and conditions of the scheme. In some instances it may be necessary to refer your claim to our specialist nurses, along with our panel of independent specialist advisors, who will advise on the level of cover available for the recommended treatment.
Duplicate cover
You must tell us if you are able to make a claim for the cost of any of your treatment from anyone else either under another healthcare scheme or under an insurance policy. For example, if you received an injury that was caused by someone else such as a road traffic accident in which you are not at fault, the scheme will only pay a share of the total costs as appropriate.
If benefits are claimed for treatment to you when the injury or medical condition was caused by a third party, the scheme shall, at its own expense, have the right to pursue such claims in any way considered appropriate in your name. You must co-operate with all reasonable requests in this respect and advise us of any amount you recover directly from the third party.
Healix privacy notice
If you would like to know more about how Healix store and process your personal data, please find our Privacy Notice by clicking here.
Section 9: Glossary
The words and phrases below have the following meanings. They will appear in bold in this guide.
Active treatment
Acute condition
Annual renewal date
Benefit
Benefits
Biological therapies
Cancer
Chronic condition
Complementary practitioner
- Acupuncture practitioners must be registered with the BMAS (British Medical Acupuncture Society), BacC (British Acupuncture Council), AACP (Acupuncture Association of Chartered Physiotherapists) or AAC (The Association of Acupuncture Clinicians)
- Osteopaths must be registered with the GOsC (General Osteopathic Council)
- Chiropractors must be registered with the GCC (General Chiropractic Council) <
Daycase
Dependant
-a member’s unmarried dependent children
Dependants
-a member’s unmarried dependent children
Dialysis
- haemodialysis, (through the use of a kidney machine or dialyser)
- peritoneal dialysis (by introducing fluid into the abdomen to act as a filter). <
Disorder
Emergency
Employer
End of life care
Gender Dysphoria
Gender Incongruence
General Practitioner
GP
High dependency unit
High risk activities
Home healthcare
Hospital
Private hospital - an independent hospital which can provide acute medical, surgical or psychiatric care. It must be registered under The Registered Homes Act (1984) and approved by the Healthcare Commission or any future law. It may also include a private bed in an NHS hospital.
Inpatient
Intensive care unit
Medical condition
Medically necessary
-
In accordance with professional standards of medical practice in the United Kingdom
-
Clinically appropriate, in terms of type, frequency, extent, site and duration of treatment
-
Required for reasons other than the comfort or convenience of the patient or specialist.
-
Provided at an appropriate facility, in an appropriate setting and at an appropriate level of care for the treatment of the patient’s medical condition.
-
Provided only for an appropriate duration of time.
-
No more costly than an alternative treatment at least as likely to produce the same therapeutic or diagnostic results.
<
Members
Mental health condition
Outpatient
Palliative care
Partner
Physiotherapist
Pre-existing condition
-
you have received medication, advice or treatment, or
-
you have experienced symptoms whether the condition was diagnosed or not.
<
Private ambulance
Prosthesis
Psychological therapist
-
a psychologist who is:
-
Registered with the Health and Care Professions Council (HCPC);
-
Registered with the British Psychological Society (BPS) as a chartered Psychologist
-
a therapist who is:
-
An accredited member of the British Association of Counselling and Psychotherapy (BACP); or
-
An Accredited Member of the British Association for Behavioural and Cognitive Psychotherapies (BABCP); or
-
An Accredited Member of Scotland’s Professional Body for Counselling and Psychotherapy (COSCA); or
-
A practitioner who is registered with the United Kingdom Council for Psychotherapy (UKCP)
Registered nurse
Related condition
Specialist
- a medical practitioner with full current registration with the General Medical Council or
-
a dentist with full current registration with the General Dental Council
and
-
a specialist in the treatment you are referred for (this is applicable to all specialities including anaesthetics and psychiatry)
-
has a certificate of Higher Specialist Training in their specialty that is issued by the Higher Specialist Training Committee of the appropriate Royal College or Faculty
-
is or has been a National Health Service consultant or dentist
-
has been recognised for benefit purposes as a specialist by Healix.
<
Start date
Surgical appliance
The Scheme
Practitioner
- an occupational therapist
- an orthoptist
- a speech and language therapist
- a dietician or;
- a nurse who is on the register of the Nursing and Midwifery Council (NMC) and holds a valid NMC personal identification number. <
Treatment
Treatments
Trust Deed
Trustee, Trustees
United Kingdom
Waiting Period
We, Us, Our
You, Your
Scheme
Pandemic
Epidemic
Member Zone
Member
Neurodevelopmental disorders
Contacting us
The Healix Team
We have a team of experienced case managers and nurses available to advise and help you, who can be contacted on the helpline number below:
Email: baxter@healix.com
Monday-Friday 08.00-19.00 (Excl. bank holidays)
Saturday 09.00-13.00
Telephone calls to and from our organisation are recorded for the purposes of quality and training.
Any correspondence should be sent to the following address:
Claims Administration Department
Healix Health Services
Healix House, Esher Green
Esher, Surrey
KT10 8AB
Section 9: Glossary
The words and phrases below have the following meanings. They will appear in bold in this guide.
Active treatment
Acute condition
Annual renewal date
Benefit
Benefits
Biological therapies
Cancer
Chronic condition
Complementary practitioner
- Acupuncture practitioners must be registered with the BMAS (British Medical Acupuncture Society), BacC (British Acupuncture Council), AACP (Acupuncture Association of Chartered Physiotherapists) or AAC (The Association of Acupuncture Clinicians)
- Osteopaths must be registered with the GOsC (General Osteopathic Council)
- Chiropractors must be registered with the GCC (General Chiropractic Council) <
Daycase
Dependant
-a member’s unmarried dependent children
Dependants
-a member’s unmarried dependent children
Dialysis
- haemodialysis, (through the use of a kidney machine or dialyser)
- peritoneal dialysis (by introducing fluid into the abdomen to act as a filter). <
Disorder
Emergency
Employer
End of life care
Gender Dysphoria
Gender Incongruence
General Practitioner
GP
High dependency unit
High risk activities
Home healthcare
Hospital
Private hospital - an independent hospital which can provide acute medical, surgical or psychiatric care. It must be registered under The Registered Homes Act (1984) and approved by the Healthcare Commission or any future law. It may also include a private bed in an NHS hospital.
Inpatient
Intensive care unit
Medical condition
Medically necessary
-
In accordance with professional standards of medical practice in the United Kingdom
-
Clinically appropriate, in terms of type, frequency, extent, site and duration of treatment
-
Required for reasons other than the comfort or convenience of the patient or specialist.
-
Provided at an appropriate facility, in an appropriate setting and at an appropriate level of care for the treatment of the patient’s medical condition.
-
Provided only for an appropriate duration of time.
-
No more costly than an alternative treatment at least as likely to produce the same therapeutic or diagnostic results.
<
Members
Mental health condition
Outpatient
Palliative care
Partner
Physiotherapist
Pre-existing condition
-
you have received medication, advice or treatment, or
-
you have experienced symptoms whether the condition was diagnosed or not.
<
Private ambulance
Prosthesis
Psychological therapist
-
a psychologist who is:
-
Registered with the Health and Care Professions Council (HCPC);
-
Registered with the British Psychological Society (BPS) as a chartered Psychologist
-
a therapist who is:
-
An accredited member of the British Association of Counselling and Psychotherapy (BACP); or
-
An Accredited Member of the British Association for Behavioural and Cognitive Psychotherapies (BABCP); or
-
An Accredited Member of Scotland’s Professional Body for Counselling and Psychotherapy (COSCA); or
-
A practitioner who is registered with the United Kingdom Council for Psychotherapy (UKCP)
Registered nurse
Related condition
Specialist
- a medical practitioner with full current registration with the General Medical Council or
-
a dentist with full current registration with the General Dental Council
and
-
a specialist in the treatment you are referred for (this is applicable to all specialities including anaesthetics and psychiatry)
-
has a certificate of Higher Specialist Training in their specialty that is issued by the Higher Specialist Training Committee of the appropriate Royal College or Faculty
-
is or has been a National Health Service consultant or dentist
-
has been recognised for benefit purposes as a specialist by Healix.
<
Start date
Surgical appliance
The Scheme
Practitioner
- an occupational therapist
- an orthoptist
- a speech and language therapist
- a dietician or;
- a nurse who is on the register of the Nursing and Midwifery Council (NMC) and holds a valid NMC personal identification number. <
Treatment
Treatments
Trust Deed
Trustee, Trustees
United Kingdom
Waiting Period
We, Us, Our
You, Your
Scheme
Pandemic
Epidemic
Member Zone
Member
Neurodevelopmental disorders
Scheme Year 2025
The new scheme year will renew on 1st January 2025. There will be no changes to the scheme for this year.
Scheme Year 2024
The new scheme year renewed on the 1st January 2023. There have been no changes made to the scheme for this year.
Scheme Year 2023
The below changes will come into effect for the new scheme year from 1st January 2023.
| New Benefits | Benefit Limit | Benefit Wording |
|
Perci Health - virtual cancer support |
Please refer to Member Zone for further information |
Please refer to your cancer support explained |
|
Digital Triage |
Please refer to Member Zone for further information |
Please refer to Musculoskeletal health pathway. |
| Benefit Changes | Previous Wording | New Wording |
|
Women's Health Benefit Remote advice service with our in-network specialist gynaecologists (up to 4 consultations per scheme year) Diagnostic tests and investigations following referral from our in-network remote gynaecologists (up to £500 per scheme year) |
Remote advice service with our in-network specialist gynaecologists We will pay for up to 4 remote advice appointments per scheme year with our in-network specialist gynaecologists on self-referral. This service can be used to discuss any women’s health concern including conditions that are normally excluded for cover such as the menopause or for contraception/fertility advice.
Diagnostic tests and investigations following referral from our in-network gynaecologists We will pay up to £500 per scheme year for diagnostic tests or investigations that are recommended following a remote advice appointment with our in-network specialist gynaecologists. Remote consultations and diagnostic tests and investigations will be covered up to the limits described above only. Once the benefit limits have been reached the scheme rules will apply as detailed in your exclusions and limitations. Please note: additional cover may be available outside of the above limits for eligible claims, please contact the claims helpline for further information. Please refer to the women's health services page for further information on how to access these benefits. |
Women's and Men's Health Benefit Remote advice service with our in-network specialist gynaecologists or men's health specialists We will pay for up to 4 remote advice appointments per scheme year with our in-network specialist gynaecologists or men’s health specialists on self-referral. This service can be used to discuss any health concern including conditions that are normally excluded for cover such as the menopause, andropause, sexual health concerns, fertility or contraception advice.
Diagnostic tests and investigations following referral from our in-network gynaecologists or men's health specialists We will pay up to £500 per scheme year for diagnostic tests or investigations that are recommended following a remote advice appointment with our in-network specialist gynaecologists or men’s health specialists. Remote consultations and diagnostic tests and investigations will be covered up to the limits described above only. Once the benefit limits have been reached the scheme rules will apply as detailed in your exclusions and limitations. Please note: additional cover may be available outside of the above limits for eligible claims, please contact the claims helpline for further information. Please refer to the women's or men's health services page for further information on how to access these benefits |
|
Outpatient consultations and diagnostic tests with a specialist on self-referral for breast, bowel or prostate cancer symptoms |
Outpatient consultations with a specialist on self-referral for breast, bowel and prostate cancer symptoms We will pay within your overall outpatient limit for self-referred consultations and investigations for breast, bowel or prostate cancer symptoms. If a diagnosis of cancer is made, cover for eligible treatment will be subject to any limits as detailed in your cancer treatment benefit. |
Outpatient consultations with a specialist on self-referral for breast, bowel, prostate and testicular cancer symptoms We will pay within your overall outpatient limit for self-referred consultations and investigations for breast, bowel, prostate or testicular cancer symptoms. If a diagnosis of cancer is made, cover for eligible treatment will be subject to any limits as detailed in your cancer treatment benefit. |
Scheme Year 2022
The below changes will come into effect from 1st January 2022
Scheme Year 2021
The below changes will come into effect for the new scheme year from 1st January 2021
| Exclusion Changes | Old wording | New wording |
|
Ageing, menopause and puberty |
Treatment to relieve symptoms commonly associated with or caused by ageing, puberty or other natural physiological cause. |
We do not pay for treatment to relieve symptoms commonly associated with or caused by ageing, puberty or other natural physiological cause. Please note: We will pay for remote consultations related to women’s health concerns with a specialist gynaecologist as specified in your table of benefits |
| New benefit | Benefit wording | Benefit limit |
|
Outpatient consultations and diagnostic tests with a specialist on self-referral for breast cancer symptoms |
We will pay within your overall outpatient limit for self-referred consultations and investigations for breast cancer symptoms. If a diagnosis of breast cancer is made, cover for eligible treatment will be subject to any limits as detailed in your cancer treatment benefit. |
Full cover |
|
Remote consultations with our in-network specialist gynaecologists for women’s health concerns |
You can contact our virtual GP, TrustDoc24, directly on 0345 319 4129 at any time to arrange a remote consultation with a GP with additional training in women’s health. Alternatively contact our helpline and speak with the nursing team, and if appropriate we may be able to arrange a remote consultation directly with our in-network gynaecologist. Please contact us to discuss this. Please note: remote consultations with our in-network gynaecologist will be limited to 4 per scheme year. If further consultations are required, these will be subject to the general terms and conditions of the scheme. There is no limit placed on remote consultations with our virtual GP. Please refer to the women’s health services page for further information on how to access this benefit. |
4 remote consultations per scheme year, via our in-network specialist gynaecologists |
|
Diagnostic tests and investigations in relation to women’s health concerns |
We will pay up to £500 per scheme year for diagnostic tests or investigations that are recommended following a remote consultation with our in-network specialist gynaecologists. Please refer to the women’s health services page for further information on how to access this benefit. |
Up to £500 per scheme year |
Scheme Year 2020
The below changes will come into effect for the new scheme year from 1st January 2020
| Wording Changes | Old wording | New wording |
|
Congenital exclusion |
Treatment for abnormalities which you have had from birth, whether or not these were diagnosed or evident at birth.
|
We do not pay for treatment for conditions which were diagnosed or evident at birth |
|
Cosmetic Treatment exclusion |
We do not pay for any form of plastic or reconstructive surgery, or scar revision, even when required for psychological reasons. We will not pay for breast enlargement or reduction or any treatment or procedure to change the shape or appearance of your breast(s) whether or not it is required for medical or psychological reasons, for example backache or enlarged breasts in males. We do not pay for any treatment, including surgery,
Exception: We will pay for post-traumatic or post-surgical reconstruction to restore function or appearance if it is medically necessary as a direct result of you having an accident or because of other surgery or cancer, which itself would have been covered under the scheme. We will pay for breast reduction/augmentation in a healthy breast if the primary purpose is to improve symmetry following surgery for cancer in the contralateral breast |
We do not pay for any treatment to change your appearance even when required for psychological reasons. We do not pay for any treatment, including surgery:
Exception: We will pay for medically necessary treatment to restore your appearance in the following circumstances:
Please note: we use NHS guidance as a benchmark for deciding whether requests for treatment are eligible for cover. All requests for cover must be submitted in writing with supporting medical information |
|
Transplant exclusion |
We do not pay for any transplants and/or complications related to, or resulting from transplants. We also do not pay for
Exception: we will pay for recipient costs for skin or corneal grafts when eligible for benefit. |
We do not pay for any transplants, adoptive cell transfer, gene therapies and/or any complications related to, or resulting from these treatments. This includes, but is not limited to CAR T cell therapy, Tumour Infiltrating Lymphocyte therapy and stem cell/bone marrow treatments.
|
|
Cancer surveillance |
You will be covered for medically necessary follow-up tests and specialist consultations needed to monitor your condition. Follow-up tests and consultations are covered for a maximum period of ten years from your last cancer treatment, in line with current clinical guidance. |
You will be covered for medically necessary follow-up tests and specialist consultations needed to monitor your condition. No time limit is placed on follow-up care for cancer, as long as it is medically necessary and we receive written confirmation of this from your specialist. |
|
General Exclusions |
The following exclusions will be removed from the scheme: AIDS / HIV Chiropody and foot care Telephone Consultations |
|
| New benefit | Benefit wording | Benefit limit |
|
Cancer outpatient therapies and cancer alternative therapies |
We will pay up to the benefit limit for physiotherapy, osteopathy, chiropractic treatment, manual lymphatic drainage and dietician services. We will reimburse up to £250 on a pay and claim basis within the above combined limit of £1,000 per scheme year for acupuncture, reflexology, aromatherapy and homeopathy. Benefits will be paid to you on receipt of the necessary documents, which must be submitted within six months of your treatment date. These benefits are available when recommended by your specialist and required as a direct result of eligible cancer treatment. Treatment must be taken with a practitioner we recognise for benefit purposes. |
We will pay a combined limit of £1,000 per scheme year for cancer outpatient therapies and cancer alternative therapies. |
|
Cancer outpatient mental health treatment |
We will pay up to £1,000 per scheme year for outpatient mental health treatment. Mental Health treatment must be with a Psychological Therapist or Psychiatrist for this to be eligible for cover. This benefit is available when recommended by your specialist and required as a direct result of eligible cancer treatment. |
We will pay up to 10 sessions per scheme year for outpatient mental health treatment. |
|
Cancer additional services |
We will pay in full for the cost of external prosthesis, wigs and medical tattooing for reconstructive purposes only. For wigs and medical tattooing benefit is available on a pay and claim basis only. Benefits will be paid to you on receipt of the necessary documents, which must be submitted within six months of your treatment date. This benefit is available when recommended by your specialist and required as a direct result of eligible cancer treatment. Treatment must be taken with a practitioner we recognise for benefit purposes |
Full cover |
Scheme Year 2019
The new scheme year has renewed on the 1st January 2019. There are no changes to the policy for this year.
May 2018
The below changes have come into affect from May 2018.
| Amendment | |
| Data Protection |
The Data Protection page has been updated in line with the new General Data Protection Regulation (GDPR) legislation that came into effect on 25th May 2018. The Data Protection page has been changed to Healix Privacy Notice. |
|
Phone Line |
The claims line is now closed on a Saturday during bank holiday weekends. The new opening hours are: Monday-Friday 08:00-18:00 (excl. bank holidays) |
Scheme Year 2018
The below changes have come into effect for the new scheme year, from 1st January 2018.
| New Benefit | Benefit limit | New benefit note |
| Virtual GP |
N/A |
As part of your Baxter Medical Scheme you have access to a virtual GP service, called TrustDoc24 which is provided by Medical Solutions. This service can be accessed 24/7, 365 days a year by phone on: 0345 319 4129, or via the app (eConsultation service is available Mon-Fri 08:00-22:00, Sat 08:00-20:00, Sun 10:00-18:00, excluding bank holidays). For further information on the service click here, and for details on how to download the app click here. Please note, during the phone call or eConsultation you will need to provide Medical Solutions with your employer’s name, Baxter, in order to access the service. Should Medical Solutions refer you onto a specialist, please contact us on your help line number 0208 763 3405 to check if this is eligible under your scheme. Any onward referrals are subject to your scheme underwriting, personal exclusions (if applicable) and general scheme exclusions. Should further information on your past medical history be required we will need your consent to contact your NHS GP. |
| Self-referred Physiotherapy |
Full Cover |
For conditions relating to muscle, bone or joint pain we will pay in full for outpatient physiotherapy without the need for a GP referral when treatment is provided by our physiotherapy network provider. We will arrange a telephone-based clinical assessment with a Senior Physiotherapist who will help organise the most effective treatment for you. This could include face to face physiotherapy, guided self-management or specialist referral. The telephone-based clinical assessment will not be subject to any excess (if one applies) however it will be applied to subsequent treatment should this be required. We will continue to monitor your progress by liaising with your treatment provider and authorise additional treatment where necessary and eligible. |
Scheme Year 2017
The below changes came into effect for the new scheme year from 1st January 2017.
| New Benefit | Benefit limit | New benefit limit |
| Wig following Cancer Treatment |
£300 per wig |
We will pay up to £300 towards the cost of a wig if you have hair loss as a result of cancer treatment. |
| Cancer Counselling Benefit |
10 sessions per scheme year |
We will cover up to 10 sessions of counselling to support any members diagnosed with Cancer. |
| Benefits wording changes |
Previous wording |
New wording |
| Preventative Treatment |
You are not covered for any preventative treatment. |
If you are being treated for cancer we may pay for medically necessary genetically-based tests to evaluate future risk of developing further cancers, as well as the resulting prophylactic surgery if it is recommended by your specialist. Please see Cancer Cover Explained for further details. |
Section 9: Glossary
The words and phrases below have the following meanings. They will appear in bold in this guide.
Active treatment
Acute condition
Annual renewal date
Benefit
Benefits
Biological therapies
Cancer
Chronic condition
Complementary practitioner
- Acupuncture practitioners must be registered with the BMAS (British Medical Acupuncture Society), BacC (British Acupuncture Council), AACP (Acupuncture Association of Chartered Physiotherapists) or AAC (The Association of Acupuncture Clinicians)
- Osteopaths must be registered with the GOsC (General Osteopathic Council)
- Chiropractors must be registered with the GCC (General Chiropractic Council) <
Daycase
Dependant
-a member’s unmarried dependent children
Dependants
-a member’s unmarried dependent children
Dialysis
- haemodialysis, (through the use of a kidney machine or dialyser)
- peritoneal dialysis (by introducing fluid into the abdomen to act as a filter). <
Disorder
Emergency
Employer
End of life care
Gender Dysphoria
Gender Incongruence
General Practitioner
GP
High dependency unit
High risk activities
Home healthcare
Hospital
Private hospital - an independent hospital which can provide acute medical, surgical or psychiatric care. It must be registered under The Registered Homes Act (1984) and approved by the Healthcare Commission or any future law. It may also include a private bed in an NHS hospital.
Inpatient
Intensive care unit
Medical condition
Medically necessary
-
In accordance with professional standards of medical practice in the United Kingdom
-
Clinically appropriate, in terms of type, frequency, extent, site and duration of treatment
-
Required for reasons other than the comfort or convenience of the patient or specialist.
-
Provided at an appropriate facility, in an appropriate setting and at an appropriate level of care for the treatment of the patient’s medical condition.
-
Provided only for an appropriate duration of time.
-
No more costly than an alternative treatment at least as likely to produce the same therapeutic or diagnostic results.
<
Members
Mental health condition
Outpatient
Palliative care
Partner
Physiotherapist
Pre-existing condition
-
you have received medication, advice or treatment, or
-
you have experienced symptoms whether the condition was diagnosed or not.
<
Private ambulance
Prosthesis
Psychological therapist
-
a psychologist who is:
-
Registered with the Health and Care Professions Council (HCPC);
-
Registered with the British Psychological Society (BPS) as a chartered Psychologist
-
a therapist who is:
-
An accredited member of the British Association of Counselling and Psychotherapy (BACP); or
-
An Accredited Member of the British Association for Behavioural and Cognitive Psychotherapies (BABCP); or
-
An Accredited Member of Scotland’s Professional Body for Counselling and Psychotherapy (COSCA); or
-
A practitioner who is registered with the United Kingdom Council for Psychotherapy (UKCP)
Registered nurse
Related condition
Specialist
- a medical practitioner with full current registration with the General Medical Council or
-
a dentist with full current registration with the General Dental Council
and
-
a specialist in the treatment you are referred for (this is applicable to all specialities including anaesthetics and psychiatry)
-
has a certificate of Higher Specialist Training in their specialty that is issued by the Higher Specialist Training Committee of the appropriate Royal College or Faculty
-
is or has been a National Health Service consultant or dentist
-
has been recognised for benefit purposes as a specialist by Healix.
<
Start date
Surgical appliance
The Scheme
Practitioner
- an occupational therapist
- an orthoptist
- a speech and language therapist
- a dietician or;
- a nurse who is on the register of the Nursing and Midwifery Council (NMC) and holds a valid NMC personal identification number. <